Whether you’ve received a referral for a mammogram or are exploring your options on your own, we’re here to help you understand what comes next. This page covers everything you need to know about a mammogram—from how to prepare beforehand, to what to expect during the exam, and how to proceed afterward.
What is a Mammogram?
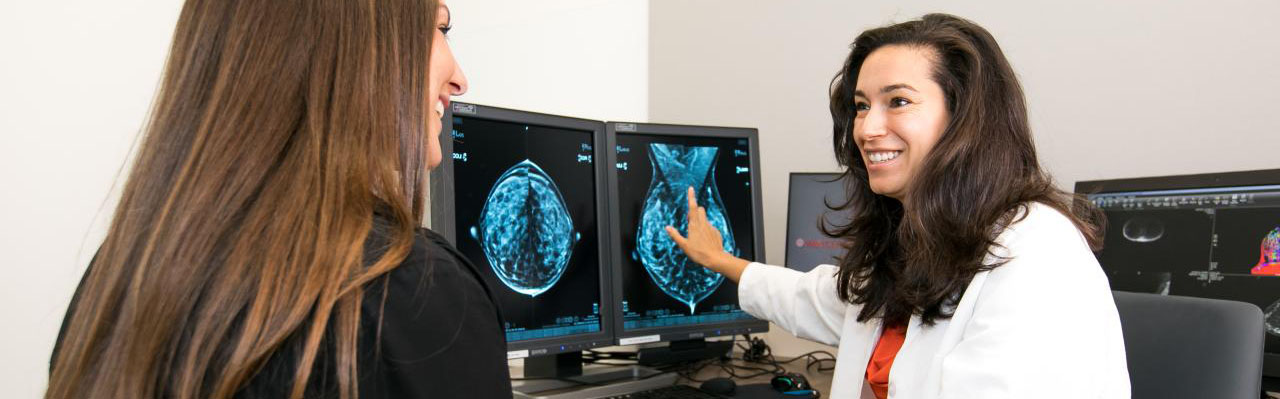
A mammogram is a low-dose X-ray exam of the breast that helps detect early signs of breast cancer, often before symptoms appear.
At WCINYP, we offer 3D mammography (breast tomosynthesis), which takes multiple images of the breast from different angles to create more detailed images.
Mammograms can indicate when further testing, like a biopsy, may be needed.
Types of Mammograms
- Screening Mammogram: Recommended for women with no symptoms. It helps detect changes that may be cancerous, often before they can be felt.
- Diagnostic Mammogram: Used when there are symptoms like a lump, pain, or nipple discharge, or to follow up on an abnormal screening mammogram.
Mammogram Guidelines
The American Cancer Society recommends the following screening guidelines for early detection of cancer in women who have no symptoms:
- Age 40 and older: Schedule a screening mammogram every year.
- Ages 20-39: Have a clinical breast exam every 3 years as part of your regular health checkup.
- High-risk individuals (family history or genetic risk): Talk to your doctor about starting screenings earlier or having them more frequently.
Screening recommendations vary based on your personal and family history. Your doctor can help you decide what’s best for your health.
Before Your Appointment
Scheduling Your Exam
Our Patient Access Coordinators are available to assist with scheduling your appointment.
(212) 746-6000
Monday through Friday, 8AM to 7PM ET, and Saturday and Sunday, 9AM to 5PM ET.
Our Locations that Offer Mammography
- Iris Cantor Women’s Health Center (Midtown East)
- Lower Manhattan
- Long Island City
Complete Your Forms Easily
Log in to Weill Cornell Connect to complete your safety forms ahead of time using eCheck-In. It’s quick and helps save you time on the day of your appointment.
Don’t have an account? Join today!
Preparing for Your Exam
When scheduling and checking in for your appointment, please let our staff know if any of the following apply:
- You have breast implants.
- You need an interpreter in your language.
FAQ
During Your Appointment
How is Mammography Performed?
- You will be comfortably positioned at the mammography unit, seated or standing.
- A paddle will gently press against each breast for about 7 to 10 seconds per view.
- You may be asked to briefly hold your breath while the X-rays are taken.
- If you feel any discomfort during the exam, notify your technologist right away.
After the Scan is Completed
The technologist will escort you to your locker to collect your belongings. Our staff will assist you with check out.
After Your Appointment
Aftercare
- You may resume all regular activity unless otherwise directed by your physician.
Imaging Review
Once the technologist has taken your images, a dedicated breast radiologist will review the images and write a detailed report. Our radiologists specialize in imaging for specific areas of the body, ensuring you receive the highest-quality, expert interpretation every time. Our specialties include:
- Abdominal
- Breast
- Cardiothoracic (Heart and Chest)
- Molecular
- Musculoskeletal
- Neuroradiology (Brain, Head, Neck and Spine)
- Pediatrics
If your screening mammogram shows something that needs a closer look, you may be called back for additional imaging. This doesn’t necessarily mean something is wrong. We just want to get a clearer view to be as thorough as possible.
Receiving Your Results
Your report will be automatically shared with you and your referring provider within 24-48 hours. You can view your images and reports through Connect. Use this guide to get started.
Sharing Your Results
All imaging exams performed at Weill Cornell Imaging will be available to you in Connect. If you'd like to keep other members of your care team informed, you can easily share your results with any additional providers.
For other medical records requests, visit our Medical Records page.
Understanding Your Results
Please contact your referring provider to discuss your results. They will help explain your imaging report and answer any questions you may have.
If you or your provider have additional questions, our Reading Room Coordinators (RRC) will help connect you with a radiologist.
For more information or to contact a RRC, visit this link.